is difficult to pass through a square or a park in South American metropolises without “El Libertador” Simón Bolívar, his sword aloft and on his bronze horse. But who remembers Arnoldo Gabaldón? The Venezuelan epidemiologist battled malaria maps, field, quinine and armies of crop-dusters laboratories door to door, so that Venezuela became a pioneer of the eradication of malaria in densely populated areas.
Gabaldon would be sweating in bed today. Half a century later, Venezuela has once again become a breeding ground of malaria, but also of communicable as HIV/AIDS or the Zika miseries. Neglected diseases such as diphtheria or measles ravage. Leprosy, tuberculosis and typhoid fever returned, along with new viruses spread by mosquitoes as dengue fever, the Zika and the chikunguna. New HIV cases grew 24 percent between 2010 and 2016.
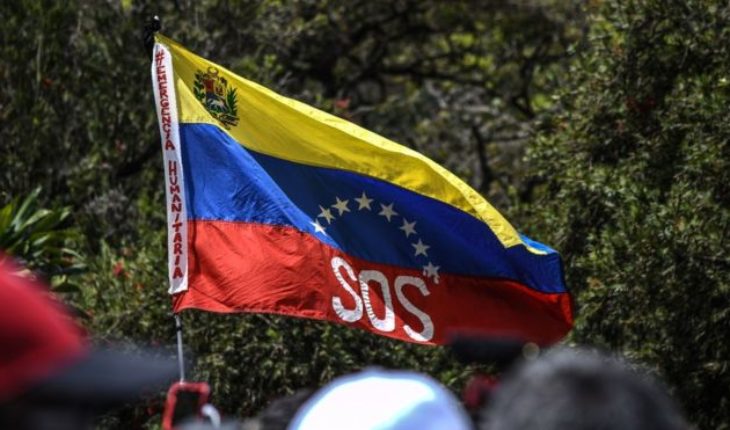
Now, the worst humanitarian crisis in America runs the risk of becoming an emergency for the hemisphere, to almost 3 million refugees and migrants Venezuelan carry their pathogens across the continent.
The poor health of Venezuela is not surprising: the disastrous Government of Nicolás Maduro has made a mess of the economy and national infrastructure. The supply shortages and blackouts in series have devastated hospitals, where nurses are forced to manually ventilate intubated patients and reuse disposable surgical gloves. One-third of Venezuelan doctors have left the country from 2014, according to the Venezuelan medical Federation.
To that, add the cost of global human stupidity: severe flooding, probably related to the disruptive climate change, have forced Venezuelans to store water in their homes; a perfect breeding ground for aedes aegypti, the mosquito that spreads dengue, chikunguna, yellow fever and the Zika. By 2016, the four types of dengue circulating throughout the country. Funding per person for populations at risk of contracting malaria in Venezuela was the youngest of America after Peru and French Guiana. So bad is the basic care that the pregnant Venezuelan prefer to risk their lives and flee the Bolivarian Republic soon to give birth in their country.
But when migrants travel, they also carry diseases that residents of Venezuela thought that they had already defeated. After recording a case of measles between 2008 and 2015, Brazil reported over 10,000 infections last year. Most of the patients suffered from measles genotype D8, the dominant strain in Venezuela. The Venezuelan epidemic has also been linked to outbreaks in Argentina, Colombia, Ecuador and Peru.
The World Health Organization estimates that an outbreak of malaria in Venezuela was responsible for 84 percent of the increase in infections in America in 2017. Venezuela itself accounted for 53 per cent of all cases reported at the regional level in 2016 and 2017.
“The human exodus has been an exodus of disease. The contagion is one of our most prolific exports”, said infectious disease pathologist Venezuelan Alberto Paniz-Mondolfi, Member of the National Academy of medicine in Venezuela. Like many of his colleagues who work in precarious conditions, Paniz-Mondolfi improvises. To speak with me, had to go to a clinic in Central Venezuela that operates natural gas, a refuge in a country beset by power outages.
Fortunately, residents of Venezuela are better prepared to deal with dangerous outbreaks. In recent decades, many have made progress in the fight against the debilitating and deadly diseases. However, the Venezuelan collapse has also left to professionals of health in the darkness; the Ministry of health stopped publishing its once respected Bulletin of health in 2016. For residents of Venezuela, its demise implies that the evaluation and treatment of refugees is a deadly Riddle.
“We see cases of brain disease at the border with Brazil which appear to be viral, but nobody knows for sure,” says Aileen Chang, researcher of Arboviruses in the George Washington University medical school, who has studied the crisis Venezuelan. “For malaria, take blood and parasites is sought in the microscope. When you have a virus is not known to what is or what it does, and there is a cheap and fast method to diagnose, there is no preparation”.
Dealing with viruses like dengue fever is particularly problematic. Spread by mosquitoes with a high degree of adaptability that breed in clean and quiet waters, biting day and flourish in populated neighborhoods, dengue travels easily and it is beautifully well adapted to the chaotic urban Latin America. Six epidemics hit Venezuela between 2007 and 2016, compared with 4 epidemics in the previous 16 years, according to a recent study in The Lancet Infectious Diseases.
The statistical blackout of Venezuela and the chronic under reporting of infections also means that increasingly frequent outbreaks point to a larger threat. “Mosquitoes are moved a few hundred meters in her life; but the people travel hundreds of kilometers if walking, thousands if they travel by boat, bus or plane,”says Donald Shepard, the Heller School of the Brandeis University Health Economist.
The worst thing is that many people — including the majority of those affected by dengue fever and up to 80 percent of those affected by the malaria – carrying the disease but don’t get sick. “When people move to take the virus with them, even without knowing it”, said Duane Gubler, an expert in new infectious diseases and Professor Emeritus of the school of medicine Duke-NUS in Singapore. “The virus mutate to pass through humans, which sometimes increases the ability of the virus and creates potential epidemiological”.
Therefore, comes as no surprise that the dengue and malaria have broken out on the border with Colombia, a no man’s land where the outlaws roam, the illegal miners looking for gold and then their profits and their infections are carried home, and the resistance guerrillas as the Colombia revolutionary armed forces and the National Liberation Army roam. “It’s a difficult place to work as a doctor or health worker,” said Martin Llewellyn, who studies disease propagated by vectors in the University of Glasgow. “It’s a wound open right in a critical border.”
When the contagion spreads, so too does the misery. Dengue cost only US$ 1842 million globally in 2016 – double that in 2013 – due to deaths, ill health, disability, treatment and rehabilitation, Shepard discovered in a recent study. And Venezuela even reached into the 10 most affected countries.
Fortunately, scientific advances are generating new promising tools. A dengue vaccine is in advanced clinical trials phase, and is working in mosquitoes that carry the bacterium Wolbachia, which inhibits the virus. However, the science alone will not stop the virus. “The best tool for mosquito control can be deployed in a country without health infrastructure and will not be enough,” said Gubler. “The problem of refuge could disappear in a few years, but the real problem – the movement of viruses and infections through the modern transport – will be there.”
In summary: the dysfunctionality of Venezuela has become an export that threatens life and poses a risk to stability and regional prosperity. “We are doctors, academics and researchers.” No we can invoke invasions or international intervention”, says Paniz-Mondolfi. “But without infrastructure, medical supplies or electricity, we cannot do our work. The authorities of the world must recognize the emergency in Venezuela until become a continental tragedy”.
The positive side is that diplomacy in America is more robust than ever, and almost all the neighbors of Venezuela are pushing mature regime to make aside, allow more humanitarian aid and will alleviate the suffering. Let us hope that they are successful: the best monument that Latin America could build to Arnoldo Gabaldón is the restoration of the legacy that built in their homeland.
translated from Spanish: The Venezuelan health crisis becomes hemispheric
April 11, 2019 |