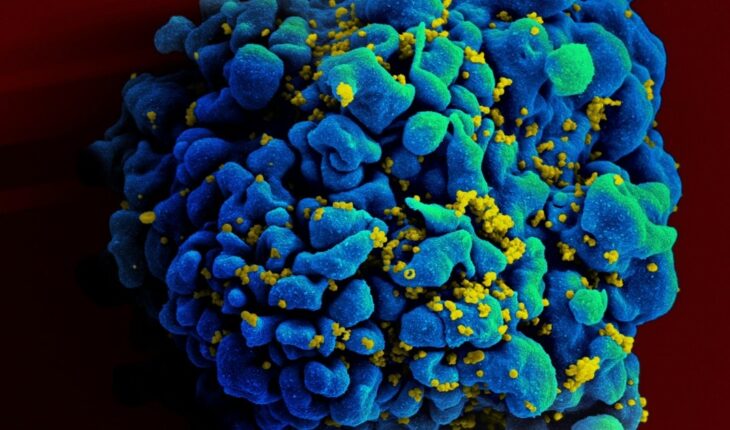
Today, HIV remains one of the biggest challenges to global public health. In our country alone, it is estimated that there are 136 thousand people who have the virus, with 17% of them unaware of it; and globally, at the end of 2020, an estimated 37.7 million people were living with HIV. In this context, various research teams as well as those working on drug development have been looking for cures and new treatment modalities for more than 40 years, but are limited by their understanding of how the virus establishes infection in the human body. How does this small virus of just 12 proteins and a genome only one-third the size of SARS-CoV-2, hijack the body’s cells to replicate and spread through systems? This is what an interdisciplinary team from Northwestern University (United States) sought to answer.
The HIV test is the only way to know if a person has contracted the virus and is done through a blood test. In Argentina it is free, voluntary and confidential.
In a new study published April 1 in the journal Nature Communications, scientists used a new approach to identify human genes that were important for HIV infection in the blood, finding 86 of them that may play a role in how the virus replicates and causes disease. included more than 40 that had never been tested in the context of HIV infection. The study proposes a new map to understand how HIV integrates into our DNA and establishes chronic infection. To do this, they isolated T cells, the main cell type targeted by HIV, from donated human blood, and removed hundreds of genes using the CRISPR-Cas9 gene-editing technique. They then infected those cells with HIV and tested them. “With the CRISPR system, there are no intermediaries — the gene is turned on or off,” said study co-author Judd Hultquist. “This ability to turn genes on and off in cells isolated directly from human blood is a game-changer: this new assay is the most faithful representation of what happens in the body during HIV infection that we could easily study in the lab.”
CRISPR/Cas9 technology is a tool for “editing” or “correcting” the genome of any cell. It would be something like molecular scissors that are able to cut any DNA molecule doing it in a very precise and controlled way.
To try to be clearer, this process of turning genes on or off is part of what is known as gene regulation and is the cause that, for example, a brain cell looks and acts differently than a liver cell or a muscle cell. That is, the regulation of genes is what causes a cell to become a red blood cell, a neuron, a hepatocyte in the liver, or a muscle cell. Genes are regulated in very different and complex ways, and modifying how that happens, then, gives rise to changes that can serve to treat diseases, create transgenic foods, improve human characteristics, among other things. Until now, studies had been based on the use of immortalized human cancer cells that, while easy to manipulate in the lab, are imperfect models of human blood cells. In addition, most of these studies used technologies to reject the expression of certain genes, but did not turn them off completely as with CRISPR, so scientists could not always clearly determine whether a gene was involved in helping or suppressing viral replication. With the new approach they were able to observe, for example, that cells that were modified to lose a gene important for viral replication showed a decrease in infection, while cells that were modified to lose an antiviral factor (proteins that constitute a first line of defense) showed an increase in infection. On the other hand, more than half (46) of these genes have never before been analyzed in the context of HIV infection, so they represent potential new therapeutic avenues for research.” Existing drug treatments are one of our most important tools in the fight against the HIV epidemic and have been incredibly effective in suppressing viral replication and spread,” Hultquist said. “But these treatments are not curative, so people living with HIV must follow a strict treatment regimen that requires continued access to good affordable health care; that simplemente is not the world we live in.” In this sense, the team is excited that CRISPR-Cas9 technology will allow us to study how it influences the independent elimination or activation of each gene involved in HIV infection to get even closer to curative strategies.